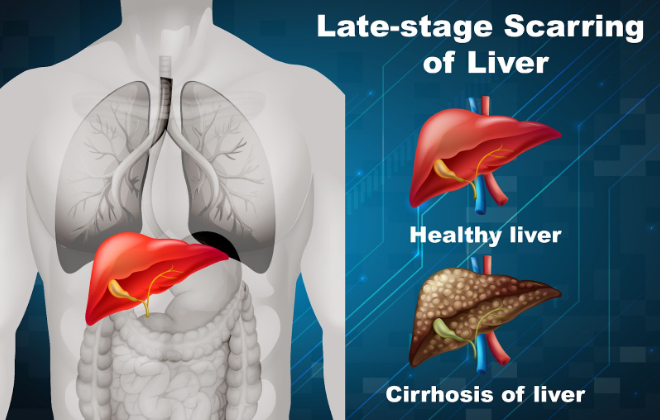
What is Liver Cirrhosis?
Liver cirrhosis is a condition in which the liver becomes severely damaged and scarred. The liver, a vital organ for detoxifying the body, producing bile, and synthesising proteins, begins to lose its functional tissue due to continuous damage. The scar tissue gradually replaces healthy tissue, which affects the liver’s ability to perform its vital functions.
Is Liver Cirrhosis Contagious?
No, liver cirrhosis is not contagious. It cannot be transmitted from person to person like a cold or flu. However, some of the conditions that lead to liver cirrhosis, such as hepatitis B or C, can be contagious. It’s important to treat the underlying conditions to prevent cirrhosis from developing.
What are the Types of Liver Cirrhosis?
Liver cirrhosis can be categorised into several types based on its causes. Understanding the type of cirrhosis you have can help determine the most effective treatment plan. The main types include:
-
Alcoholic Cirrhosis
This type is the result of long-term heavy alcohol consumption. Alcohol is toxic to the liver, and over time, it causes irreversible damage.
-
Hepatitis Cirrhosis
Chronic viral infections like hepatitis B or C can cause liver inflammation and damage, leading to cirrhosis.
-
Non-Alcoholic Fatty Liver Disease (NAFLD)
This occurs when fat builds up in the liver without alcohol consumption. It’s commonly associated with obesity, diabetes, and metabolic syndrome.
-
Biliary Cirrhosis
This type occurs when bile ducts in the liver become damaged, leading to a buildup of bile in the liver and causing scarring.
-
Autoimmune Cirrhosis
This happens when the body’s immune system attacks the liver, causing inflammation and scarring.
What are the Four Stages of Liver Cirrhosis?
Cirrhosis progresses in stages, and the severity of the disease determines the treatment options. The four stages of liver cirrhosis are:
-
Stage 1 (Compensated Cirrhosis)
At this stage, the liver still functions normally despite some scarring. Patients may not experience noticeable symptoms, but the liver is already damaged.
-
Stage 2 (Decompensated Cirrhosis)
The liver’s function begins to decline. Symptoms like fatigue, nausea, and swelling in the legs or abdomen may start to appear. Complications can arise at this stage.
-
Stage 3 (Severe Cirrhosis)
The liver is severely scarred and has a significantly reduced ability to function. Complications such as jaundice, internal bleeding, and liver failure may occur.
-
Stage 4 (End-Stage Liver Disease or Liver Failure)
The liver can no longer perform its essential functions, and patients may require a liver transplant to survive.
What are the Signs & Symptoms of Liver Cirrhosis?
Liver cirrhosis can have varying symptoms depending on its stage. Common symptoms include:
- Fatigue and weakness
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain or discomfort
- Swelling in the abdomen (ascites) or legs (edema)
- Itchy skin
- Loss of appetite and weight loss
- Nausea or vomiting
- Bruising or bleeding easily
It’s essential to pay attention to these signs and seek medical evaluation as early detection can significantly improve the prognosis.
How Does Liver Cirrhosis Occur?
Several risk factors can contribute to liver cirrhosis. These include:
- Chronic alcohol consumption: One of the leading causes of cirrhosis.
- Chronic viral infections: Hepatitis B and C can lead to cirrhosis if untreated.
- Non-alcoholic fatty liver disease (NAFLD): A result of obesity, diabetes, and high cholesterol.
- Genetic conditions, Such as hemochromatosis or Wilson’s disease.
- Autoimmune liver diseases: Conditions where the body’s immune system attacks the liver.
How is Liver Cirrhosis Diagnosed?
Liver cirrhosis diagnosis typically involves a combination of medical evaluations, blood tests, and imaging tests.
Medical Evaluations
-
Medical History
The doctor will ask about your alcohol consumption, medical history, and possible exposure to hepatitis viruses.
-
Physical Exam
The doctor may check for signs like jaundice, swollen abdomen, or enlarged liver.
Blood Tests
Blood tests are conducted to assess liver function. These tests check for elevated liver enzymes, low albumin levels, and abnormal clotting function, which can indicate liver damage.
Imaging Tests
- Ultrasound: To examine the liver’s structure.
- Fibroscan: To assess the fibrosis or scarring.
- CT Scan or MRI: To assess liver damage and complications.
- Liver Biopsy: A small sample of liver tissue may be removed for examination under a microscope to confirm cirrhosis.
What are the Treatment Methods for Liver Cirrhosis?
While there is no cure for liver cirrhosis, treatment focuses on managing symptoms, slowing disease progression, and preventing complications.
Over-the-Counter Medications and Home Remedies
- Pain relief: Over-the-counter medications like acetaminophen (Tylenol) can help with mild pain.
- Vitamins and supplements: Some patients may need additional vitamins, such as vitamin K or vitamin D, to support liver function.
Medical Treatment
- Antiviral Medications for cirrhosis caused by hepatitis B or C, antiviral treatments can slow the disease’s progression.
- Diuretics: Medications that reduce fluid retention in the body.
- Liver Transplant: In advanced stages of cirrhosis, a liver transplant may be necessary if the liver has lost most of its function.
Hospitalization
Severe complications like internal bleeding, infections, or liver failure may require hospitalisation. In such cases, doctors, including hepatologists, will provide critical care, and patients may be monitored closely.
How to Prevent Liver Cirrhosis?
Liver cirrhosis prevention is largely based on maintaining liver health and avoiding factors that can lead to liver damage. Some strategies include:
- Limit alcohol consumption: Heavy drinking is a major cause of cirrhosis.
- Vaccination against Hepatitis: Vaccinate against hepatitis B and C if at risk.
- Maintain a healthy weight: Prevent obesity and manage conditions like diabetes.
- Avoid exposure to toxins: Minimise contact with harmful chemicals or drugs that can damage the liver.
- Regular medical checkups: Regular screening and early detection of liver conditions can prevent cirrhosis from developing.
Frequently Asked Questions
Can cirrhosis be reversed?
No, liver cirrhosis is irreversible. However, with early treatment and lifestyle changes, its progression can be slowed.
What is the life expectancy with liver cirrhosis?
Life expectancy depends on the cirrhosis stage and underlying causes. With proper treatment, many people can live for years, but in advanced stages, it may be significantly reduced.
Is cirrhosis only caused by alcohol?
No, cirrhosis can also be caused by viral hepatitis, fatty liver disease, autoimmune conditions, and genetic disorders.
Can I drink alcohol if I have cirrhosis?
It is highly advised to avoid alcohol if you have cirrhosis, as it can worsen liver damage.
How can I protect my liver from cirrhosis?
Maintain a healthy diet, avoid excessive alcohol, get vaccinated against hepatitis, and manage risk factors like obesity and diabetes.
What foods are good for liver health?
Foods rich in antioxidants, fiber, and healthy fats like fruits, vegetables, and whole grains are beneficial for liver health.
Is liver cirrhosis fatal?
If left untreated, cirrhosis can lead to liver failure, which can be fatal. Early diagnosis and treatment are crucial.
Can cirrhosis be diagnosed with a blood test?
Blood tests can detect liver damage, but imaging tests and a biopsy are often needed to confirm cirrhosis.